Constipation and Anal Fissure
We are here for your care
Constipation and Anal Fissure Surgeon in Mumbai.
Expert care for constipation and anal fissure in Mumbai. Learn about causes, symptoms, and treatments for constipation and anal fissure. Consult Dr. Husain Gheewala for effective diagnosis and treatment options.
Constipation is very common and it affects people of all ages. Remember, everyone has different bowel habits, for some passing stools, 3 times a day is normal and for some passing stools 3 times a week can be normal. So, if you notice change from your routine bowel habits that would be significant.
Constipation can usually be treated at home with simple changes to your diet and lifestyle.

Constipation

It’s likely to be constipation if:
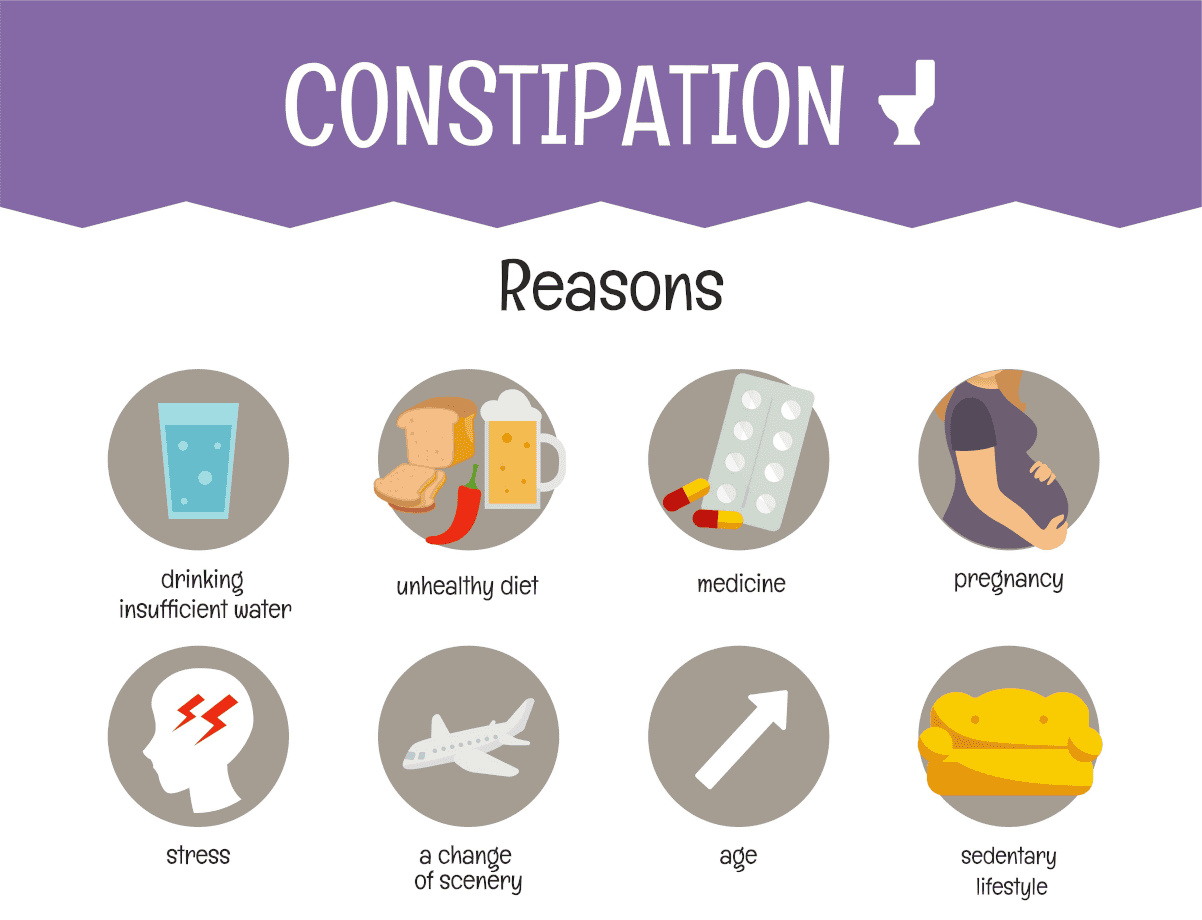
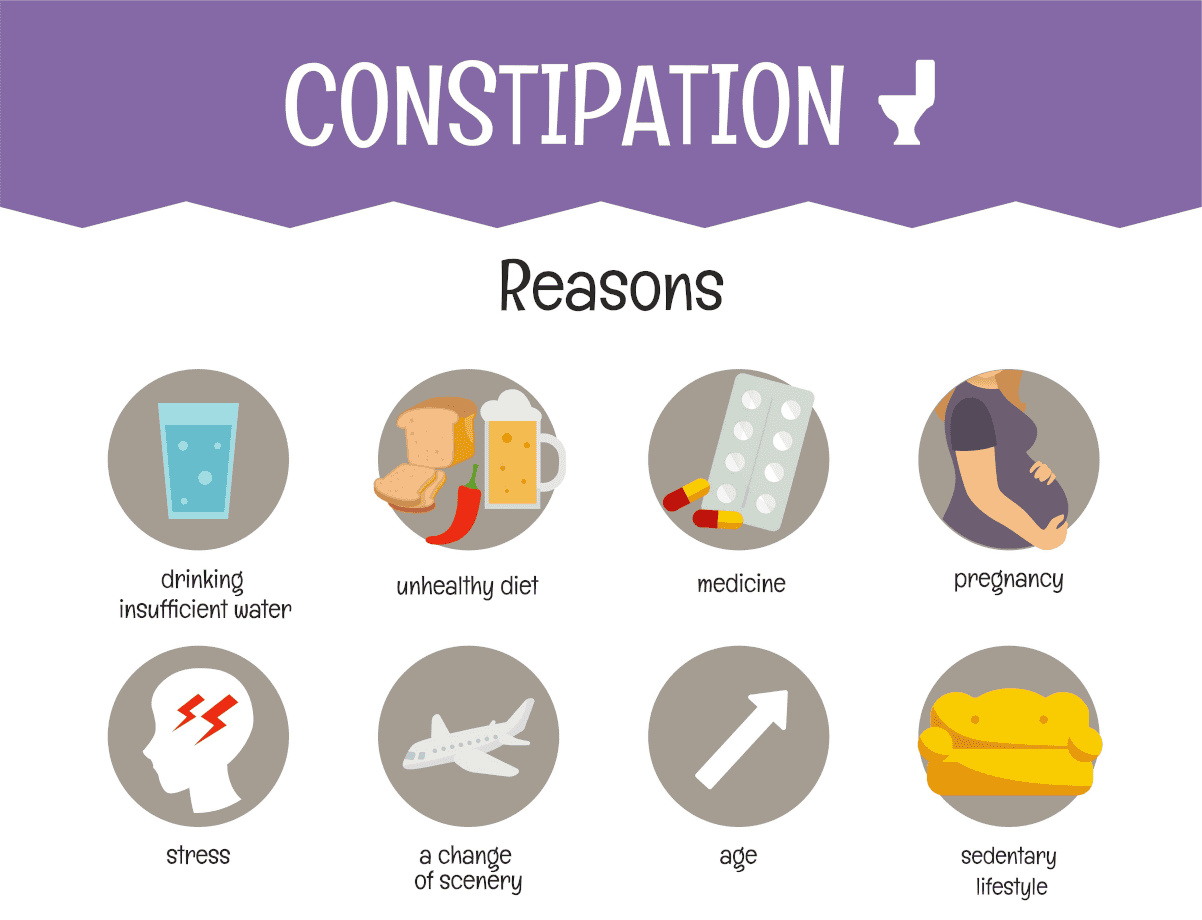
Causes
Constipation in adults has many possible causes. Sometimes there’s no obvious reason.
The most common causes include:
Constipation is also common during pregnancy and for 6 weeks after giving birth. Rarely, constipation may be caused by a medical condition

Treatment
Making simple changes to your diet and lifestyle can help you treat constipation.
You may notice a difference within a few days. Sometimes it takes a few weeks before your symptoms improve.
To make your stools softer and easier to pass:
Improve your routine
Keep to a regular time and place and give yourself plenty of time to use the toilet.
Do not delay if you feel the urge to pass stools.
Squatting position (Indian Toilet) is better position to pass stools then Sitting position (western toilets) when the stools are hard and you have to strain.
A daily walk or run can help you pass stools more regularly.

Consult a Specialist if you

Anal Fissure
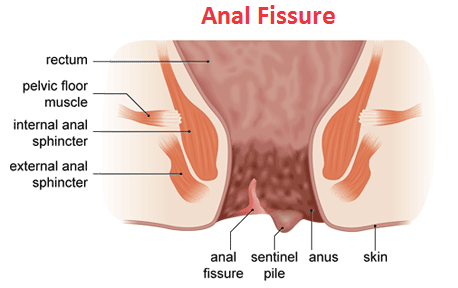
Faeces (stools) is temporarily stored in the rectum and expelled from the body via the anus (back passage). The membranous lining of the anus is called the anal mucosa. An anal fissure is a tear in the anal mucosa.
If you see blood in your stools, or have pain and discomfort in your bottom, you might have an anal fissure. An anal fissure can be very uncomfortable, but it will usually heal if you make some changes to your diet and follow some simple treatments.
Anal fissures are very common and can occur in people of all ages and genders, with around 1 in every 10 people affected at some point in their life.
They affect both sexes equally and people of all ages can get them.
But children and young adults between 10 and 30 years of age are more likely to get anal fissures.
The problem is common in children younger than one year, and affects around eight out of 10 babies. A person’s susceptibility to anal fissures tends to decline with age.
Common causes in adults include constipation and trauma to the anus (such as a difficult childbirth).
Around half of cases heal by themselves with proper self-care and avoidance of constipation. However, healing can be a problem if the pressure of passing bowel motions constantly reopens the fissure. Treatment options include medication and surgery.
Causes
Most anal fissures are caused by trauma to the area, mainly from passing a hard or large stool during a bowel movement. Other causes of anal fissures include:


Symptoms
An anal fissure can cause signs and symptoms such as:
Complications
Anal fissures aren’t associated with more serious diseases, such as bowel cancer, although cancer of the anus may mimic an anal fissure. Some of the possible complications of an anal fissure include:
Diagnosis
An anal fissure is diagnosed using a number of tests including:


Treatment
Conservative treatment usually works, taking 1 to 2 months. It involves:
Surgery
An operation is an option if the fissure fails to heal or comes back. The usual operation is to make a small cut in the muscle around the anus (internal sphincterotomy). This permanently reduces the tone (pressure) around the anus and allows the fissure to heal. This is a minor operation which is usually done as day case surgery (you will not usually have to stay overnight in the hospital). The success rate with surgery is very high. At least 9 in 10 cases are cured.Diagnosis
Botox
Botox is a chemical that is injected into the muscles around the anus to help them relax. Botox usually lasts for 2 to 3 months, which allows the fissure to heal.


