Haemorrhoids (Piles)
We are here for your care
Haemorrhoids (Piles) Doctor in Mumbai.
Looking for a Haemorrhoids (Piles) Doctor in Mumbai? Find detailed information on symptoms, causes, diagnosis, and treatment options for haemorrhoids.
Haemorrhoids, also known as piles, are swellings containing enlarged blood vessels (veins) that are found inside or around the back passage (the rectum and anus).
In many cases, haemorrhoids don’t cause symptoms, and some people don’t even realise they have them.

Haemorrhoids (Piles)

They happen when there is a weakness in the side of the anal canal that leads to thickening of the lining and then veins can enlarge within the haemorrhoid, causing symptoms such as bleeding, pain and discomfort.
They can be of 2 types, internal piles, inside the rectum, which is less sensitive to pain and irritation, or external, under the skin around the anus, which can produce symptoms.
You may also experience prolapsed haemorrhoids, which are a very painful type of haemorrhoids that originate internally. Here, veins push out through the anus and hang out of the body and may be constricted (strangled) by a ring of muscle, known as the anal sphincter.
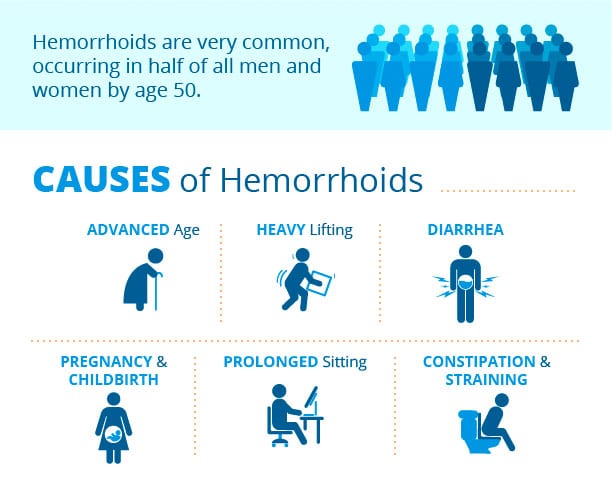
Causes
Haemorrhoids generally occur over a period of time, when small blood vessels and veins located around the anus and rectum experience certain blockages or compression. These blockages lend blood vessels and veins a swollen or knobbly appearance.
The blockages, themselves, are the result of significant pressure being applied in this area. Given their placement, these piles tend to get irritated during bowel movements.
Pressure can be built as a result of many factors, some of the most common of which include:
Haemorrhoids are particularly common during pregnancy (25%-35%) This is because constipation is quite common in pregnancy, but also:
Alongside direct causes, there are also certain risk factors that may make you more likely to develop piles. These include factors such as age, hereditary and genetic factors, weight, and the level of physical activity or exercise you get.
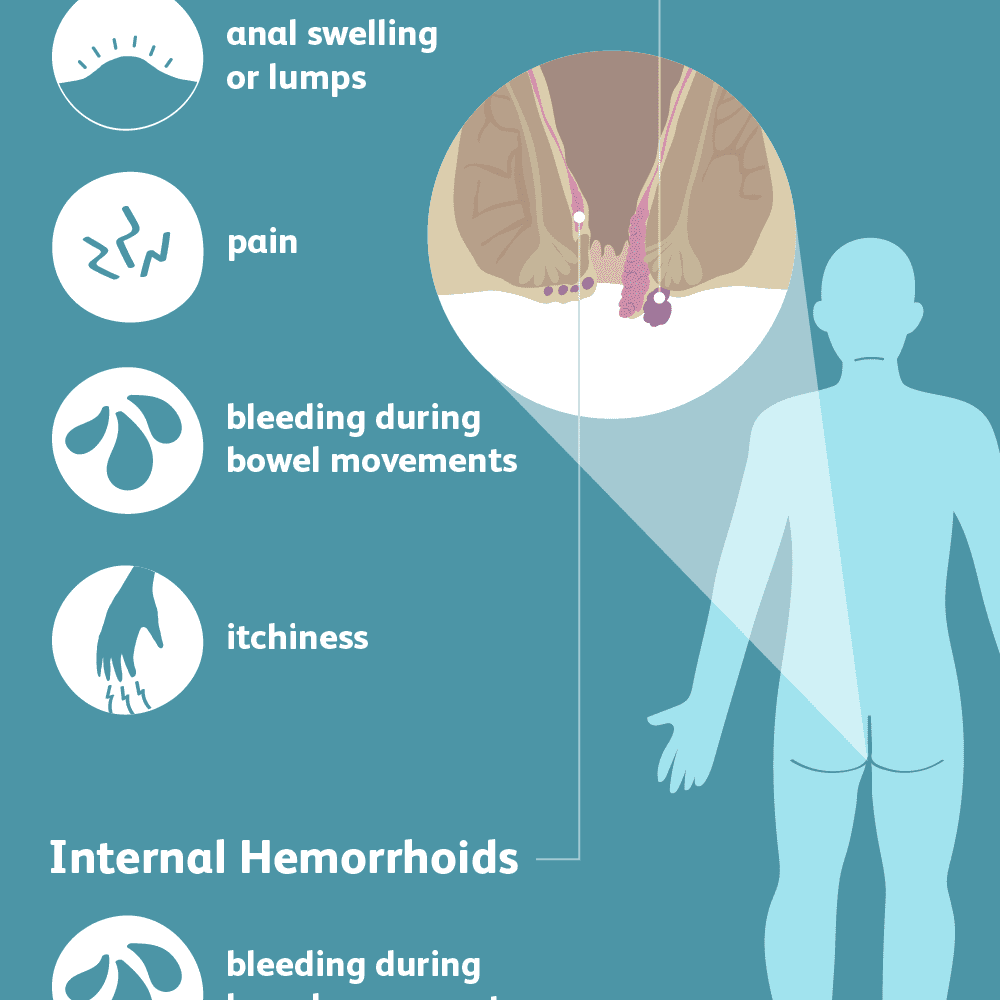
Symptoms
In many cases, haemorrhoids don’t cause symptoms, and some people don’t even realise they have them. However, it’s estimated that 60% of cases of haemorrhoids are symptomatic, when symptoms do occur, they may include:
Haemorrhoids aren’t usually painful, unless their blood supply slows down or is interrupted.
Haemorrhoids can lead to other medical conditions such as anaemia (low Hb), which takes place if there’s a significant loss of blood.
Additionally, blood clots can form inside haemorrhoids, requiring them to be drained in certain cases, especially if they cause pain.
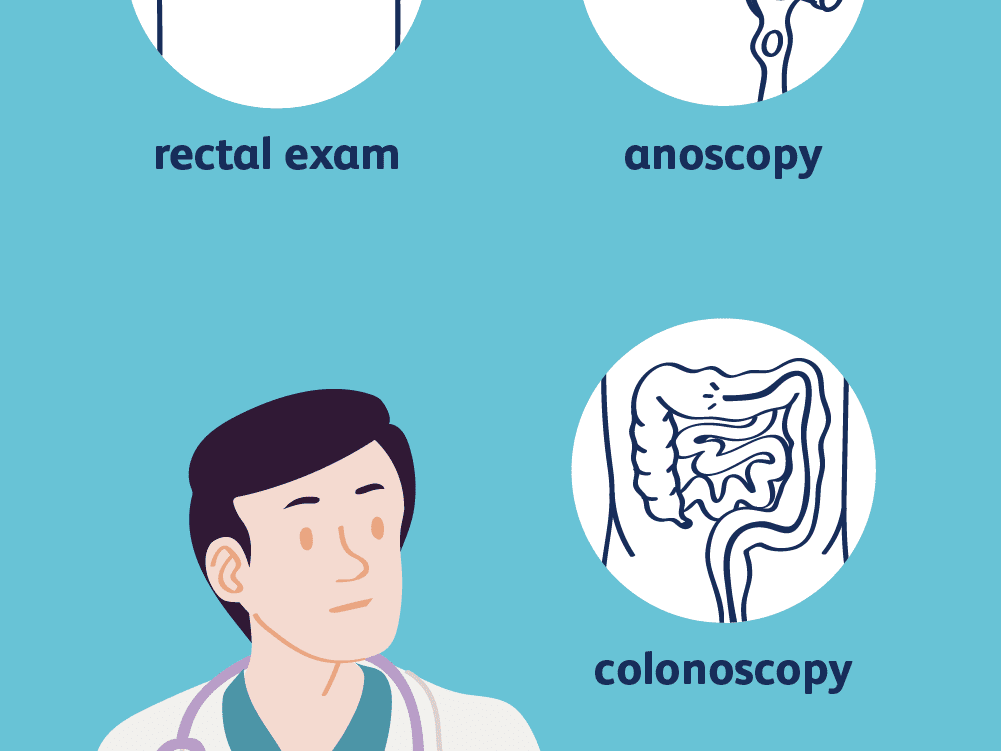
Diagnosis
Diagnosis of haemorrhoids usually involves an examination of the back passage to look for any swollen blood vessels. Following examination are usually conducted.
There is no need to feel embarrassed about these tests — haemorrhoids are a common problem and your specialist is used to diagnosing and treating them.
There may be a suggestion to get a colonoscopy (camera test to view your entire colon) depending on your signs and symptoms.


When should you see a specialist?
Haemorrhoids often go away without any treatment. However, if you notice blood when you have a bowel motion, it is important to get it checked out by a specialist, to make sure your symptoms are not a sign of something more serious. The symptoms of haemorrhoids can be very similar to bowel cancer. Please note that haemorrhoids per se are not associated with an increased risk of bowel cancer.
Tell your doctor if you have noticed:
If you are having severe signs and symptoms of haemorrhoids that is if the haemorrhoids are getting too large, if they’re causing discomfort or pain along with bleeding, if you’re having both internal and external haemorrhoids, or if they’re persisting for a long time then you should see a specialist.
Treatment options
Medications
Pain and inflammation can often be relieved using over-the-counter haemorrhoid treatments from the chemist, including medicated creams, ointments and suppositories (solid medicines designed to be inserted into the anus). Laxatives are also prescribed to keep the stools soft.
Non-surgical treatments
If dietary changes and medication don’t improve your symptoms, your specialist may recommend appropriate treatment.
If you have haemorrhoids in the upper part of your anal canal, non-surgical procedures such as banding and sclerotherapy may be recommended.
Less often, a surgical procedure called haemorrhoidectomy may be needed. Here, an operation is carried out under general anaesthetic to surgically remove the haemorrhoids.

Surgery
Although most haemorrhoids can be treated using the methods described above, around 1 in every 10 people will eventually need surgery. Surgery may be recommended if other treatments for haemorrhoids (piles) haven’t worked, or if you have haemorrhoids that aren’t suitable for non-surgical treatment.
There are many different types of surgery that can be used to treat haemorrhoids, but they all usually involve either removing the haemorrhoids or reducing their blood supply, causing them to shrink.
Haemorrhoidectomy
A haemorrhoidectomy is an operation to remove haemorrhoids. It’s usually carried out under anaesthesia, which means you’ll not feel your bottom during the procedure and won’t feel any pain while it’s carried out.
A conventional haemorrhoidectomy involves gently opening the anus so the haemorrhoids can be cut out.
You’ll probably experience significant pain after the operation, but you will be given painkillers. You may still have pain a few weeks after the procedure, which can also be controlled with painkillers.
After having a haemorrhoidectomy, there’s around a 1 in 20 chance of the haemorrhoids returning, which is lower than with non-surgical treatments. Adopting or continuing a high-fibre diet after surgery is recommended to reduce this risk.
Haemorrhoidectomy
Haemorrhoidal artery ligation is an operation to reduce the blood flow to your haemorrhoids.
Each blood vessel is stitched closed to block the blood supply to the haemorrhoid, which causes the haemorrhoid to shrink over the following days and weeks. It can also be done under Ultrasound guidance. It causes less pain and, in terms of results, a high level of satisfaction has been reported.
The recovery time after having haemorrhoidal artery ligation is also quicker compared with other surgical procedures.

Stapling
Stapling, also known as stapled haemorrhoidopexy, is an alternative to a conventional haemorrhoidectomy. It’s sometimes used to treat prolapsed haemorrhoids and is carried out under anaesthesia.
During the operation, part of the anus involving the haemorrhoids, is stapled. This means the haemorrhoids are less likely to prolapse and it reduces the supply of blood to the haemorrhoids, which causes them to gradually shrink.
Stapling has a shorter recovery time than a traditional haemorrhoidectomy, and you can probably return to work about a week afterwards. It also tends to be a less painful procedure.
Other treatments
Other treatment options are available, including freezing and laser treatment. However, the results are varying.

