Pelvic Floor Procedures
We are here for your care
Pelvic Floor Procedures Surgeon in Mumbai.
Looking for a skilled pelvic floor procedures surgeon in Mumbai? Dr. Husain Geewala offers top-notch services for pelvic floor treatments. Contact us today!
A rectal prolapse is when part of your rectum (back passage) slides out through your anus (the opening in your bottom), forming a swelling there. You may only get the rectal prolapse swelling when you’re passing stools at first, but eventually it might be there all the time.

Rectal Prolapse

Having a rectal prolapse can be very uncomfortable and interfere with your daily life. It is an embarrassing feeling, but its important to see a specialist to get the right treatment and guidance.
If you have a rectal prolapse, the most obvious symptom is having a lump or swelling coming out of your bottom. Other symptoms of a rectal prolapse may include:
Should I push a rectal prolapse myself?
If you or your child has a rectal prolapse, it may go back inside by itself at first after you’ve finished emptying your bowels. But sometimes it doesn’t, and your specialist may show you how to push it back in yourself. Always follow their advice.
Pushing a rectal prolapse back in needs to be done very gently, and you need to try and relax (or encourage your child to relax) while you’re doing it. You’ll probably find it easier to do while lying on your back or side, rather than sitting or squatting down. Press gently and steadily on the prolapsed tissue to help it go back inside through the anus (back passage). Your specialist may advise you to use a little lubricating jelly to help it slide back in more easily.
If the prolapse still won’t go back in, or it becomes painful, or you notice dark or bluish-purple tissue, you should seek medical attention as soon as possible. Don’t keep trying to push it back or you may cause damage to the wall of your bowel.
The best treatment for you will depend on the type of prolapse you have, as well as other things like your age and your overall health. In young children, especially those under the age of four, rectal prolapse usually gets better by itself, without any specific treatment.

Conservative therapy
Before trying other treatment, you might want to:
If your symptoms don’t improve, you may need surgery to secure the rectum into place.
For a full-thickness rectal prolapse, adults usually need an operation to fix it.
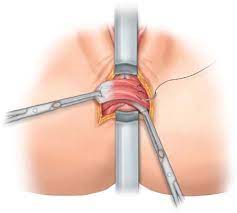
There are many different ways to surgically correct rectal prolapse.
This may be performed via the abdomen or directly on the prolapse at the anus. The decision to recommend either abdominal or rectal surgery is based on a number of factors including age, physical condition, extent of prolapse, and the results of various tests.
An abdominal repair (rectopexy) aims to lift the rectum up and fix it so that it cannot prolapse out through the anus again. For many patients, this can be performed laparoscopically (keyhole repair of the prolapsed bowel). The repair is often reinforced with mesh to get the best long-term results. The most modern version of this operations is done Robotically.
Dr. Gheewala has been trained in both Laparoscopic and Robotic Surgery for Rectal Prolapse in the UK. His experience in the field has helped many patients deal with such condition.
Anal Incontinence Treatment
Anal or faecal incontinence can be a very debilitating disease. It is a condition where one loses control over their back passage and it can be of different types. There can be accidental loss of solid stools to liquid stools to accidental loss of flatus (Gas).
There are many causes of faecal incontinence, but most common are with disorders of the anal sphincter (the anal sphincter is a ring of muscle that controls the exit of faeces out of your body) and pelvic floor. Injuries may occur following vaginal delivery, or other anorectal trauma (trauma to back passage). Other causes include radiation to the pelvis, inflammatory bowel disease, behavioural and neurological abnormalities.
Treatment depends on the cause, and hence multiple investigations are carried out.
Management often involves many different approaches.
Some of these are outlined here:

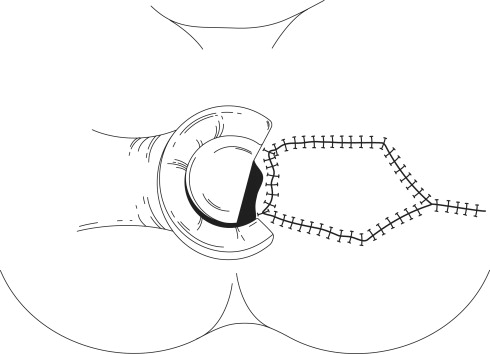
Sphincter Repair
This procedure is carried out when the muscle of the anal canal, or sphincter has been torn. This injury most often occurs through vaginal delivery of childbirth. The tear may have been recognised at the time of delivery and repaired, or may not have been obvious, and thus not diagnosed. Also, sphincters can be damaged if surgeries around your back passage gets complicated.
Repair of the sphincter requires a cut through the perineum (region around your bottom), and dissection between the anus and vagina. The ends of the sphincter muscle are dissected then sutured together. It requires experience and training to perform these repairs.
Providing there are no complications, surgery will improve symptoms in 7 to 8 out of 10 people if they have had no major problems with bowel control. It is important to understand that control of gas and liquid stool may not be perfect and that you may still have some urgency, especially if your bowels are loose.
Anal Stenosis
Anal stenosis, which is a narrowing of the anal canal (back passage) that makes it difficult to pass stools, can lead to serious complications if left untreated. Also referred to as anal stricture, this condition occurs when the muscles in the anus—which expand and contract to regulate the passage of faecal material—becomes narrow or tight.
In the majority of cases, anal stenosis is linked to scar tissue formation, which can occur after trauma or any surgery in the anal region (back passage). Other possible causes of anal stenosis include:
The symptoms of anal stenosis might seem minor at first, but they can worsen with time. They include:
The non-surgical treatment options for anal stenosis are limited, though fibre supplements, stool softeners, laxatives may help.
Depending on the severity of the condition, surgery may be an option.
Common surgical options include an anoplasty (correcting the damage in the sphincter muscle), which is the surgical reconstruction of the anus, or a sphincterotomy, which involves the cutting of the internal sphincter muscle to reduce tension. These treatment approaches and many others are offered by Dr. Gheewala.
Pilonidal Sinus
A pilonidal sinus is a small hole or tunnel in the skin at the top of the buttocks, where they divide (the cleft).
Most people with a pilonidal sinus do not notice it unless it becomes infected and causes symptoms.
An infection will cause pain and swelling, and a pus-filled abscess can develop.
In most of the people there are multiple opening as seen in the above pic, there can be infection in these sinuses leading to pus/abscess formation.
It’s very important to keep the area between your buttocks clean by showering or bathing regularly.
Certain factors increase the risk of developing the condition and include:


Treatment
In most cases, an operation will be advised. There are various operations which are done to cure this problem. Your Specialist Surgeon will be able to give the details and the advantage and disadvantages of each operation.
The options include the following:
