Inflammatory Bowel Disease(IBD) and Diverticulitis
We are here for your care
Inflammatory Bowel Disease(IBD) and Diverticulitis Surgeon in Mumbai.
Looking for a skilled Diverticulitis Surgeon in Mumbai? Dr. Gheewala provides expert treatment for Diverticular Disease. Learn about symptoms, causes, and treatments here.
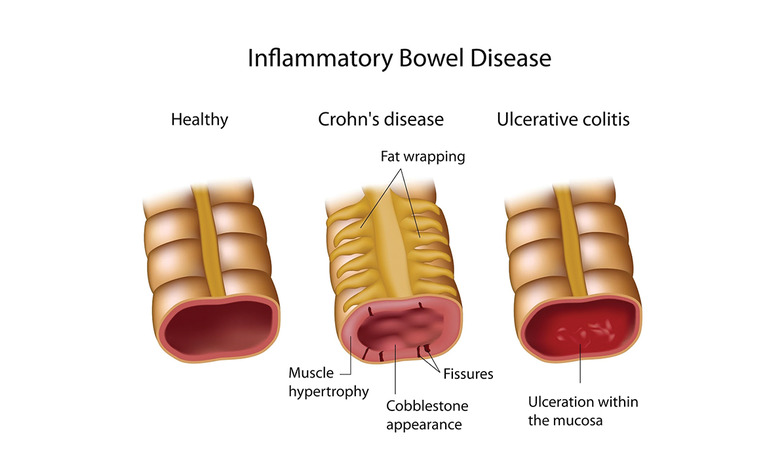
When one talks about inflammatory bowel disease it usually means people who either have Crohn’s Disease or Ulcerative Colitis. Both these conditions can cause inflammation of the colon and rectum (large bowel or large intestine) with similar symptoms, such as pain in abdomen, bloody diarrhoea, etc.

Inflammatory Bowel Disease
They’re usually the result of an infection near the anus causing a collection of pus (abscess) in the nearby tissue.
When the pus drains away, it can leave an opening behind.
Ulcerative colitis, in which inflammation is limited to the surface layers of the large bowel (colon).
Crohn’s disease, which can occur anywhere in the digestive tract from the mouth to the anus (back passage), and which causes inflammation of the entire thickness of the intestinal wall.
Some people are diagnosed with ‘indeterminate colitis’, when their inflammatory bowel disease cannot be distinguished between ulcerative colitis and Crohn’s disease.
Ulcerative colitis is the most common type of inflammatory disease of the bowel.
IBD can first present at any age but the most common age is between 15-30 years. There is a second smaller peak age for symptoms to start between 50-70 years.
Crohn’s disease is more likely in those with a strong family history (first-degree relative affected, i.e., parent, brother or sister) and in people who smoke.
Infections (especially upper respiratory and bowel infections) or taking non-steroidal anti-inflammatory drugs (NSAIDs) can also aggravate symptoms.
Causes
It’s unclear what causes IBD, but it’s thought to be caused by a combination of factors, including:
- genetics – you’re more likely to get IBD if you have a close relative with the condition
- a problem with your immune system. It seems that the body’s immune system is triggered by factors such as bacteria or viruses to cause inflammation in the gut (bowel) wall.
People who smoke are twice as likely to get Crohn’s disease than non-smokers.
There is some evidence that living in urban or industrialised areas may increase Crohn’s disease risk, possibly due to differences in diet, gut microbes or the effect of pollution.
Symptoms
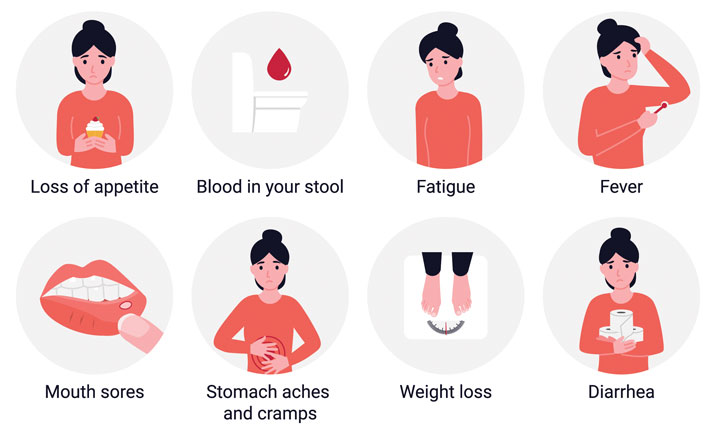
The symptoms are very variable depending on severity and which part of the gut (bowel) is affected. The symptoms of IBD can come and go. There may be times when the symptoms are severe (a flare-up), followed by long periods when there are few or no symptoms at all (remission).
The symptoms may include:
- Tummy (abdominal) pain and cramps.
- Diarrhoea (may be bloody).
- Urgent need to open your bowels.
- High temperature (fever).
- Weight loss.
- Loss of appetite
- extreme tiredness
However, the symptoms are very variable, not everyone has all these symptoms, especially for people with Crohn’s disease, which can affect any part of the gut (bowel).
Damage to the intestinal wall leads to ulceration and bleeding. People with Crohn’s disease can also experience:
- Narrowing (strictures) of the bowel
- Breaks (perforation) of the bowel
- Tunnels between sections of the bowel or other organs (fistulae)
These complications require medical and sometimes surgical treatment.
The inflammation in Crohn’s disease and colitis is not limited to the intestine. People often experience problems caused by inflammation in other organs including their eyes, skin, liver and joints.
In the long-term, people with inflammatory bowel disease are at elevated risk of bowel cancer.
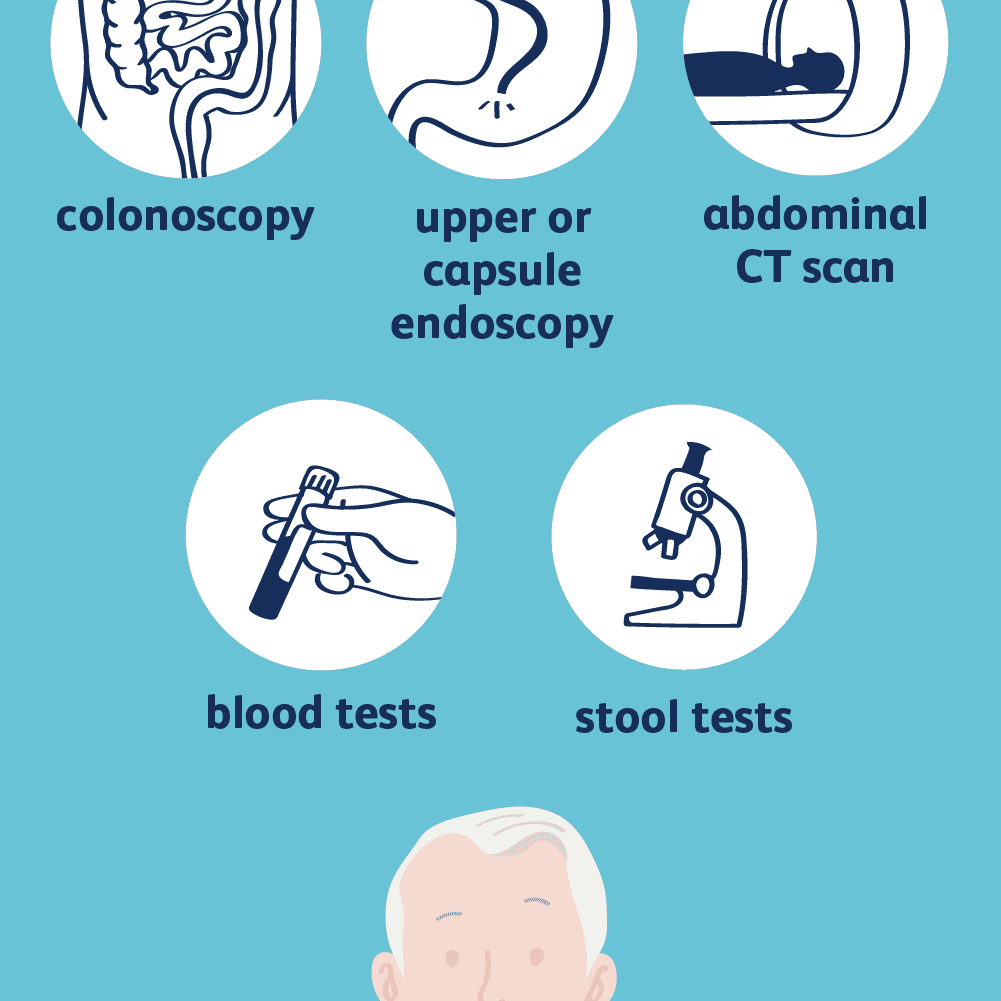
Diagnosis
If you have symptoms that suggest the possibility of inflammatory disease then you should see a specialist, you may be advised to do the following test which may include:
- Blood test, including a full blood count to check for anaemia and a blood test to check for any indication of inflammation. The main tests for inflammation are called erythrocyte sedimentation rate (ESR) and C-reactive protein (CRP).
- Stool tests to check whether there is any infection in your gut (bowel) or any blood in your gut.
- Scans, may be suggested such as CT and MRI scans.
- Sigmoidoscopy and or Colonoscopy (Camera test of you large bowel) to look at the lining of your large bowel (colon) and to take biopsies may be suggested.
Based on the results of the test, you may be advised accordingly.
Complications
- Persistent blood loss causing anaemia.
- Rupture of the bowel wall (perforation).
- Narrowing of the bowel causing obstruction (stricture), more common with Crohn’s disease.
- Ulceration and abnormal passages (fistulae) around the back passage (anus).
- Severe dilatation of the large bowel (colon). This is called toxic megacolon and is more common with ulcerative colitis than Crohn’s disease.
- Reduced absorption of food from bowel causing malnutrition.
- Increased risk of bowel cancer (especially ulcerative colitis).
- Stoma formation (ileostomy or colostomy) – this may be needed after an operation to remove part of the bowel.
Treatment
For most people, inflammatory bowel diseases are lifelong illnesses. Treatment aims to relieve the symptoms and prevent them from returning, and includes specific diets, lifestyle changes, medicines and surgery.
Treatments for people with inflammatory bowel disease may include:
- Medications, such as steroids, to reduce inflammation
- ‘Biologic’ medications that block the specific molecules that allow inflammation to occur
- Antibiotics
- Surgery to remove areas of severe inflammation, or to repair damage.
It’s estimated that 1 in 5 people with ulcerative colitis have severe symptoms that do not improve with medicine. In these cases, surgery may be necessary to remove an inflamed section of large bowel (colon). Around 60 to 75% of people with Crohn’s disease will need surgery to repair damage to their digestive system and treat complications of Crohn’s disease.
If you have mild ulcerative colitis, you may need minimal or no treatment and remain well for prolonged periods of time. For people with severe ulcerative colitis, the entire large bowel can be surgically removed. This can be done laparoscopically or using Robotic Surgery. This cures the disease, but other health issues can remain. Crohn’s disease cannot be cured.
Dr. Gheewala has been trained in the UK for performing such complex surgeries.
Dietary modification is sometimes recommended for people with inflammatory bowel disease. Nutritional deficiencies are common, especially when inflammation is present, so adequate nutrition is important.
Diet
Changes to your diet may help to reduce your symptoms. The dietary advice will depend on your symptoms and it’s essential to make sure you get enough energy and nutrients from your diet. Therefore, it’s very important to discuss any dietary advice with your doctor or with a dietician. This dietary advice may include reducing the amount of fibre in your diet and eating small regular meals.
A low-residue diet may also be used for IBD. This is a very restricted diet with less fibre. This diet can help to reduce symptoms such as diarrhoea and pain but needs supervision by a dietician. You will need to take vitamin supplements because a low residue diet doesn’t contain all the nutrients you need.
Managing Stress
Stress can make your symptoms worse so it’s very important to learn how to manage stress. The ways we manage stress vary from person to person but meditation and regular exercise will help.


Diverticulitis
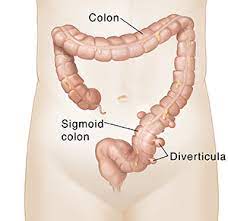
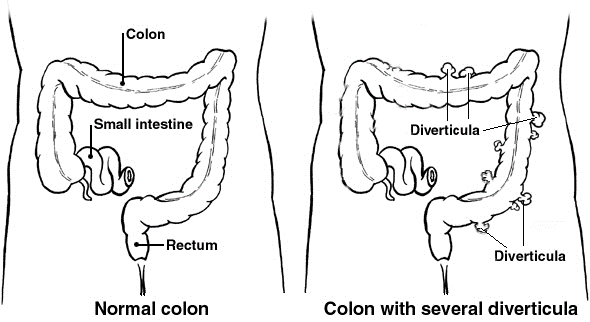
Diverticula are small bulges or pockets that can develop in the lining of the intestine as one gets old.
A diverticulum is a small pouch with a narrow neck that sticks out from (protrudes from) the wall of the gut (intestine). ‘Diverticula’ means more than one diverticulum. They can develop on any part of the gut but usually occur in the colon (sometimes called the large bowel or large intestine). This is where the stools (faeces) are becoming more solid. They most commonly develop on the left-hand side of the tummy (abdomen). Several diverticula may develop over time. Some people eventually develop many diverticula.
It is more common in ‘Western’ nations including North America, UK, Europe and Australia. It is less common in Asia and very uncommon in Africa.
Most people with diverticula do not get any symptoms and only know they have them after having a scan for another reason.
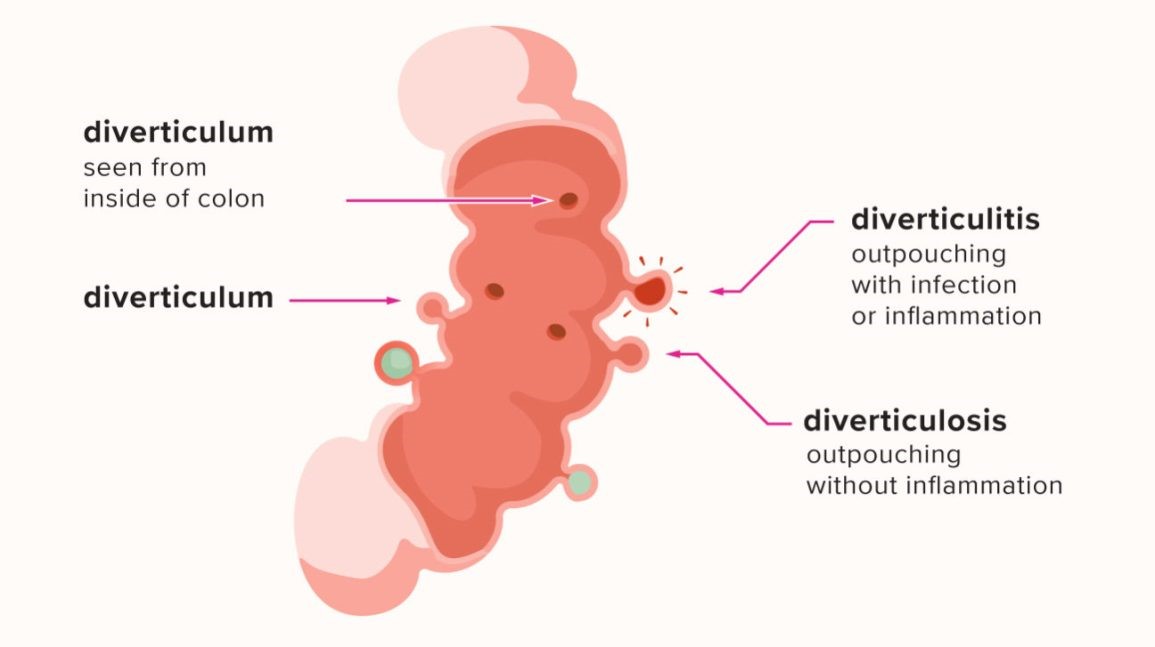
When there are no symptoms, it is called diverticulosis.
When diverticula cause symptoms, such as pain in the lower tummy, it’s called diverticular disease.
If the diverticula become inflamed or infected, causing more severe symptoms, it’s called diverticulitis.
You’re more likely to get diverticular disease and diverticulitis if you do not get enough fibre in your diet.
Causes
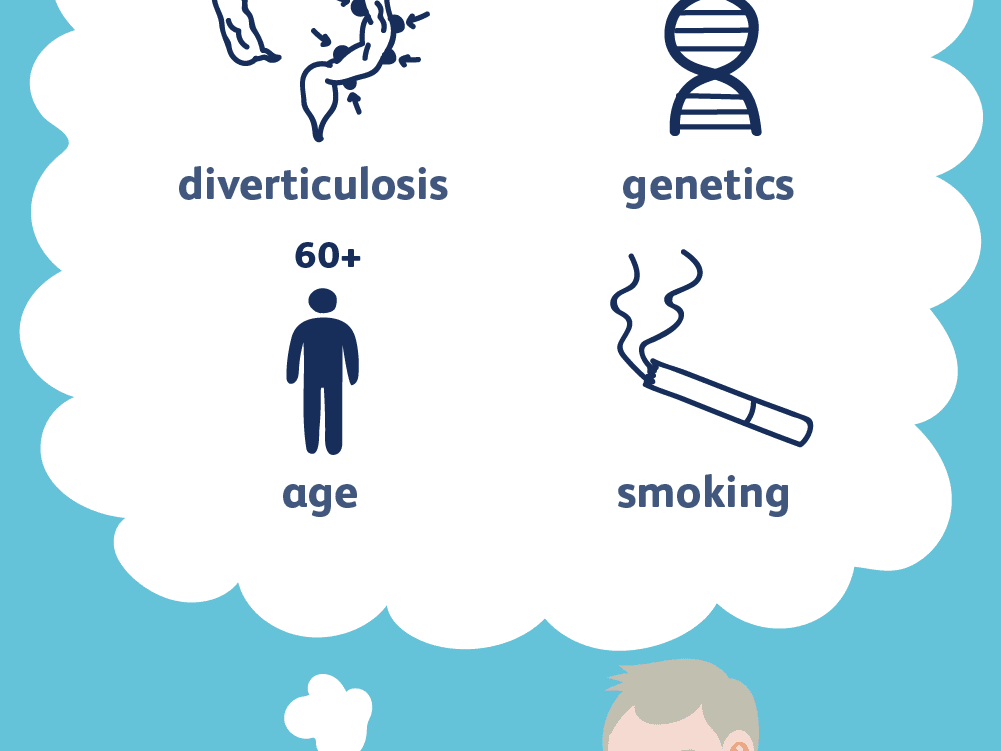
It’s not known exactly why some people get diverticular disease, but it seems to be linked to age, diet and lifestyle, and genetics.
- Age
As you get older, the walls of your large intestine become weaker and the pressure of hard stools passing through your intestines can cause diverticula to form.
The 7 out of 10 people will have some diverticula by the time they’re 80 years old.
- Diet and lifestyle
Not eating enough fibre is thought to be linked to developing diverticular disease and diverticulitis.
Fibre helps to make your stools softer and larger so they put less pressure on the walls of your intestines.
Some other things that seem to increase your risk include:
- smoking
- being overweight
- having a history of constipation
- long-term regular use of painkillers such as ibuprofen or aspirin
- Genetics
You’re more likely to develop diverticula if you have a close relative with diverticular disease, especially if they developed it before they were 50.
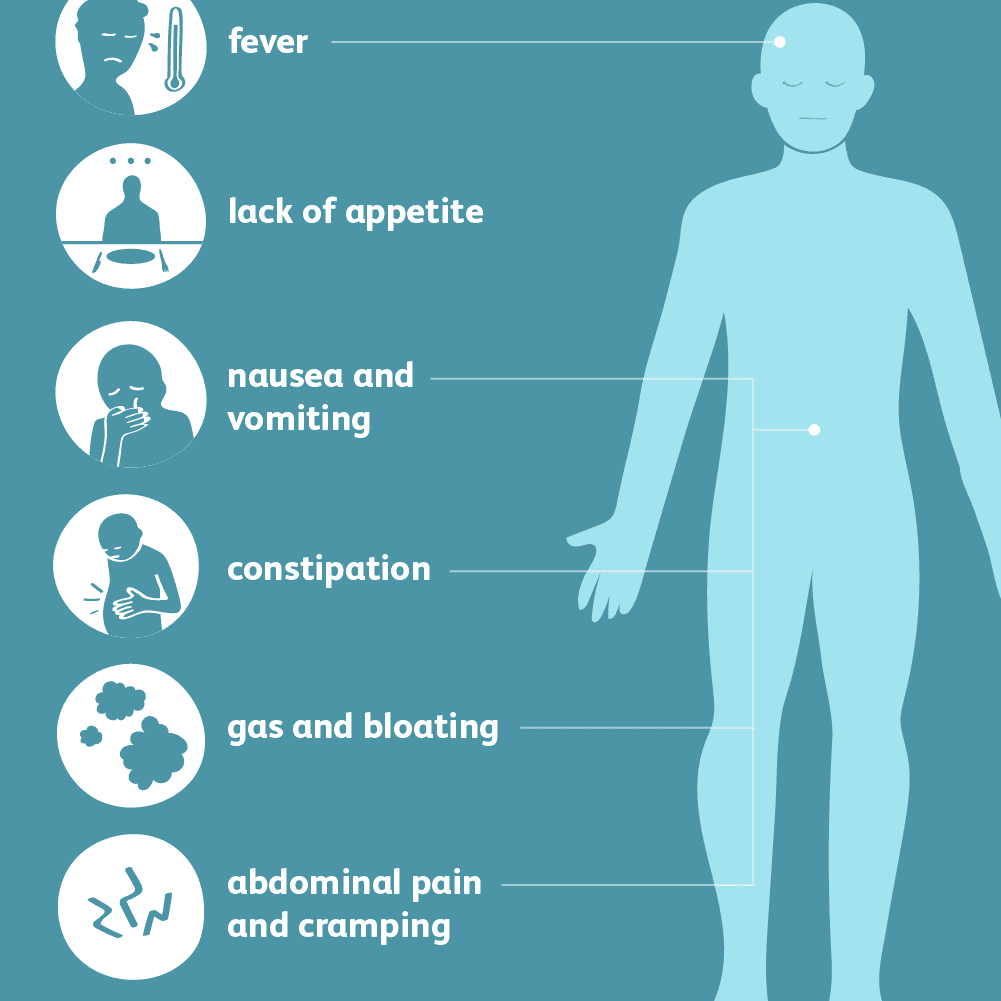
Symptoms
In about 3 in 4 people who develop diverticula, the diverticula cause no harm or symptoms.
Symptoms of diverticular disease include:
- tummy pain, usually in your lower left side, that tends to come and go and gets worse during or shortly after eating (passing stools or farting eases it)
- constipation and/or diarrhoea
- occasionally, blood in your stools
If your diverticula become infected and inflamed (diverticulitis), you may suddenly:
- get constant, more severe tummy pain
- have a high temperature
- have diarrhoea or constipation
- get mucus or blood in your stools, or bleeding from your bottom.
When to get Medical Help?
Contact a specialist as soon as possible if you have symptoms of diverticular disease or diverticulitis.
If you have any bleeding or severe pain, seek immediate medical advice.
- Tests for diverticular disease and diverticulitis
After taking your medical history and listening to your symptoms, the specialist will first want to rule out other conditions, such as irritable bowel syndrome, coeliac disease, or bowel cancer.
These often have very similar symptoms to diverticular disease.
This may involve blood tests. If necessary, you’ll be referred for a colonoscopy (camera test from you back passage), a CT scan, or sometimes both.
Treatment
Diet
Eating a high-fibre diet may help ease the symptoms of diverticular disease and stop you developing diverticulitis.
Good sources of fibre include fresh and dried fruits, vegetables, beans and pulses, nuts, cereals and starchy foods.
Fibre supplements, usually in the form of sachets of powder that you mix with water, are also available.
Gradually increasing your fibre intake over a few weeks and drinking plenty of fluids can help prevent side effects associated with a high-fibre diet, such as bloating and farting.
Medicine
Mild Diverticulitis can usually be treated at home with antibiotics prescribed by a specialist.
You can take paracetamol to help relieve any pain. Do not take aspirin or ibuprofen, as they can cause stomach upsets. More serious cases of diverticulitis may need hospital treatment.
Surgery
Surgery may be needed to treat serious complications of diverticulitis. Surgery usually involves removing the affected section of your large intestine.
If complications develop
Some people with diverticulitis develop complications such as:
- Bowel blockage (obstruction).
- A collection of pus (an abscess).
- A channel (fistula) that may form to other organs.
- A tummy (abdominal) infection (peritonitis).
Surgery is usually needed to treat these serious but uncommon complications. For example, surgery is sometimes needed to drain an abscess or to remove a badly infected part of the colon.
Dr. Gheewala has operated on various complicated patients with Diverticular disease in his career especially during his work experience back in the UK.
How to Help Yourself?
Eat more fibre
Adding more fibre to your diet may help your symptoms. It can make your bowel movements more regular and encourage healthy bacteria to grow in your tummy and bowel.
Drink more fluids
If you’re eating more fibre drink lots of fluids because fibre absorbs water. Most adults should drink around 1.5 to 2 litres of fluid every day. This is roughly the same as six to eight mugs of water.
Change your lifestyle
You may also ease your symptoms if you:
- eat regular meals
- stop smoking
- lose weight
- Exercise regularly to encourage bowel function and peristalsis.
- don’t take medicines that may cause constipation for example, painkillers containing opioids

